Get to know about telehealth, the waiver 1135, Medicare guidelines, coding and documentation, private and other payers, controlled substance non-face-to-face visits and other types of visits; and understand the proper diagnosis codes for COVID related visits.
On our most recent webinar, “Getting paid for Telehealth & non-face-to-face visits during COVID-19”, Caroline Balestra, Business Process Analyst at Health Prime, talked about telehealth, phone visits and other important types of service visits covered during a public health emergency such as COVID-19. With this information, you may be able to understand ways to ensure you get paid for this type of visits.
To get started, there's a question that sometimes confuses physicians and other practitioners: Is there a difference between Telemedicine and Telehealth?
Telehealth is different from telemedicine in that it refers to a broader scope of remote health care services than telemedicine. But, more recently since the widespread use of Telehealth and Telemedicine, both terms are used interchangeably as synonymous and there is really not any difference anymore.
Public Health Emergency (PHE) – Waiver 1135
The Secretary of Health and Human Services (HHS) may temporarily waive or modify certain Medicare, Medicaid, and Children's Health Insurance Program (CHIP) requirements to ensure sufficient health care items available to meet the needs of individuals enrolled in Social Security Act programs in the emergency area and time periods.
It is also done so providers who give such services in good faith can be reimbursed and exempted from sanctions as long as they are absent any determination of fraud or abuse.
There are TWO requirements:
- The president must have first declared an emergency or disaster under either the Stafford act or the national emergencies act.
- The Secretary must have declared a public health emergency under section 319 of the public health service act.
Since this is a social security act that makes these exceptions for Medicare, commercial payers do not have to follow them. Private payers can also cooperate, but they are not required to do it.
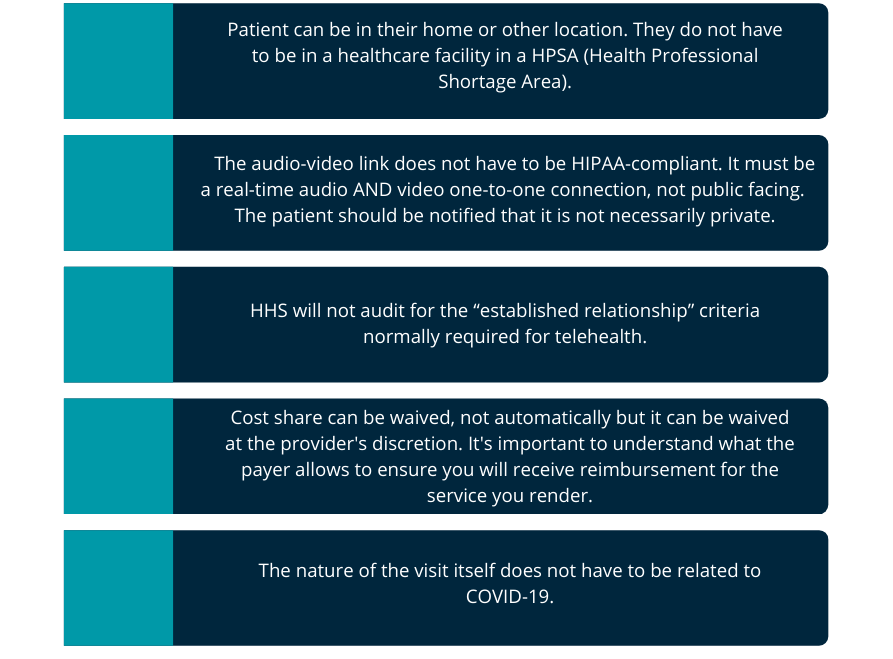
From March 6th, 2020 through the duration of the PHE:
Medicare Advantage is not Medicare!
These Medicare Advantage plans are required to offer beneficiaries at least the same benefits they receive from regular fee for service Medicare, but they function as commercial, private payers. Some will follow FFS Medicare in this, others will be more liberal in their coverage. It's important that you understand the requirements for the specific commercial Medicare advantage plan you are working with.
What are some questions you can ask to commercial payers related to telehealth coverage?
“It is essential that you ask some important questions to commercial payers so you can understand the benefit the patient plan offers. Understanding the plan benefits will allow for correct coding, submission and will help to ensure your payment for services”
-Balestra explained.
Some questions you can ask yourself are: what are the effective dates?, what services are covered?, may these services be provided by Nurse Practitioners, Physician Assistants, and other Qualified Healthcare Providers (QHP)?, how are those to be billed?, do we use telehealth codes or office visit codes?, what place of service?, what modifiers are necessary?, is this only for services related to COVID-19?
Some important things you need to know:
- Even during PHE, telehealth requires real time audio and video.
- Only services on the telehealth code list are to be used and all criteria for each CPT must be met.
- The new guidance from CMS states that the provider can choose to use whichever POS is most appropriate and apply a -95 modifier when applicable.
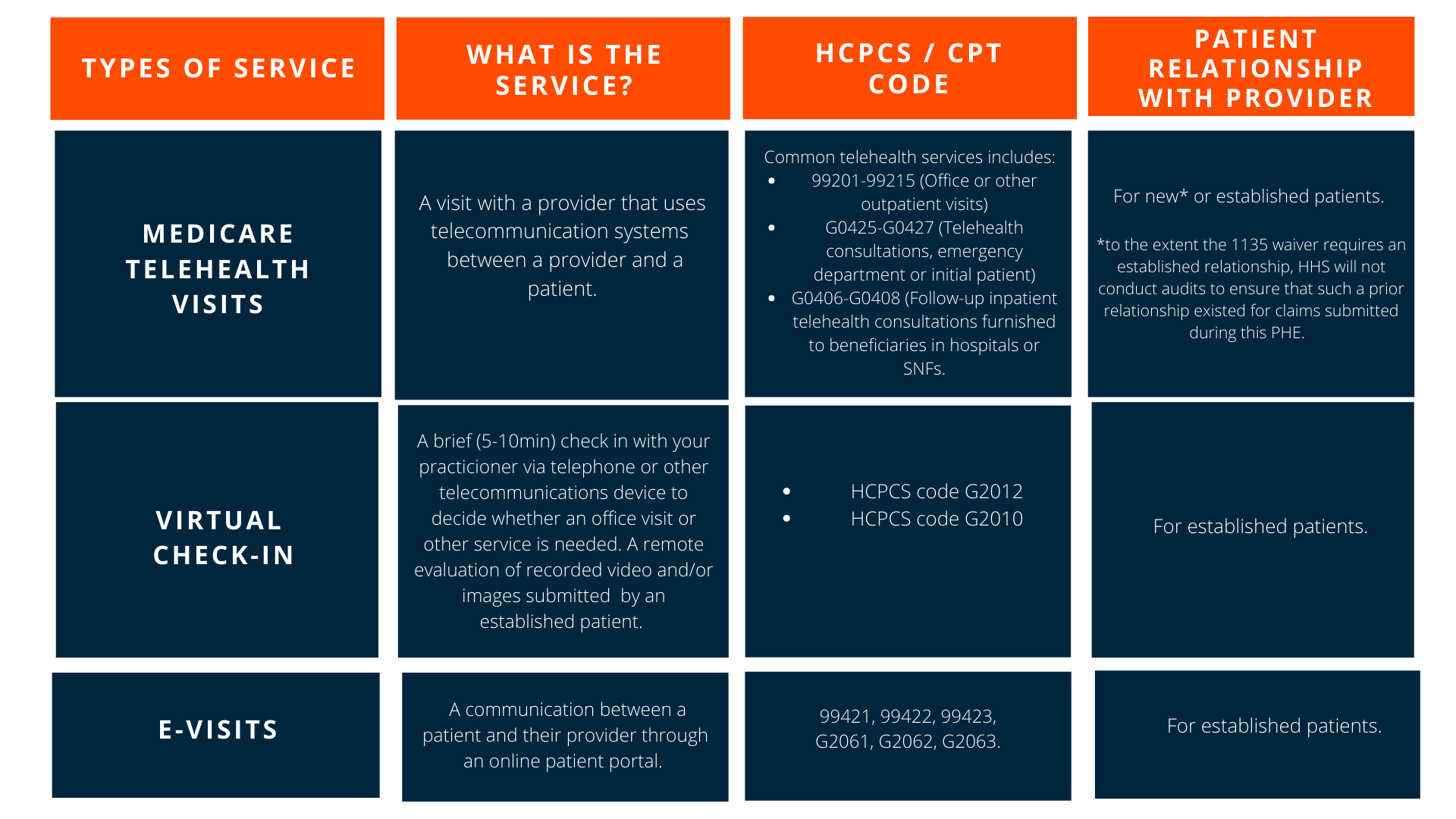
- Other services now payable such as virtual check-in, online services, and telephone calls are not considered telehealth. They are considered CTBS (Communication Technology Based Services).
What are some common modifiers for Telehealth?
- Modifiers 95: Synchronous telemedicine service that must be a live audio-video linkage connection. It cannot be “store and forward” and can be use in lieu of place of service 02.
- GQ: Asynchronous telecommunications system to be used only for patients in Alaska or Hawaii.
- GT: Via interactive audio and video telecommunications system.
- GO: used for telemedicine for symptoms of acute stroke.
The CMS stated that a modifier is not necessary when using POS 2, but there are some contractors and payers that wants you to use the modifier CR for catastrophe or disaster related services.
What happens with the CPT coding in telehealth?
Medicare has outlined that the Evaluation and Management (E/M) level selection for telehealth services can be based on MDM (Medical Decision Making) or time.
New or established CPT codes can be used and will no longer require the components that reference typical face to face time. Each service includes a medically appropriate history and/or examination. Then, the code selection will be based on the MDM level or total time spent on that date of the encounter.
Time documentation is required with this new rule. Activities included are preparation to see the patient, performing the exam, counseling, or educating the patient, caregiver, or family, ordering medications or testing, and care coordination, among a few other activities.
“How can I document an exam without laying hands on the patient?” It is possible to perform an exam just with observation and talking with a patient during a real time audio and video conference. You can analyze general appearance, sclera anicteric injected, hearing intact, skin tone, respiratory effort, gait and station, mental status and more"
- Balestra said.
Ensure that your documentation is complete, based on your MDM and that includes establishing a diagnosis, assessing the status of a condition and / or selecting a management option.
If you would like to review what is included on MDM and know more about the E/M Coding changes for 2021 in more detail, please review our What's changing for E/M codes this 2021 blog.
Private and other Payers
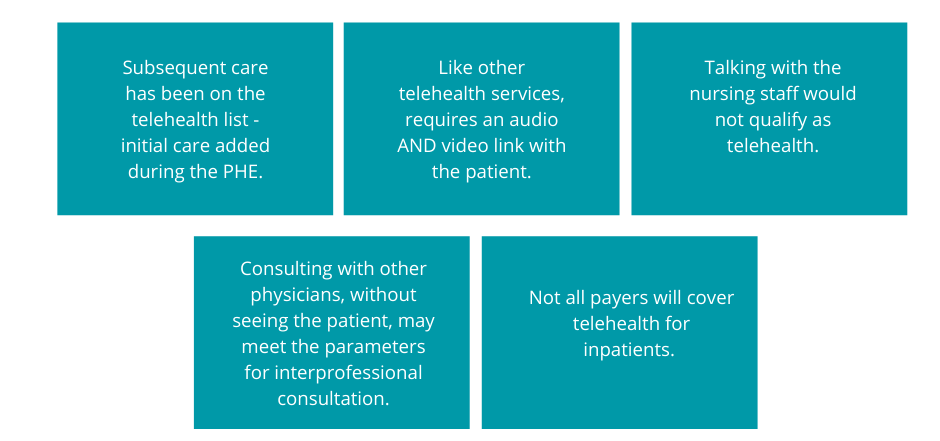
What happens in hospitals and nursing facilities?
Interprofessional Internet Consultation
This type of consultations is NOT considered as telehealth.
CMS recognizes and pays for interprofessional consults codes 99446 through 99449 and codes 99451 and 99452.
Specific CPT codes may have certain requirements including a written and/or verbal report to the requesting physician. These CPT codes can be billed but not as telehealth type of visit. You would have to use the appropriate place of service but -02 is not allowed for these as it represents telehealth.
Let's review some non-face-to-face visits that you need to consider:
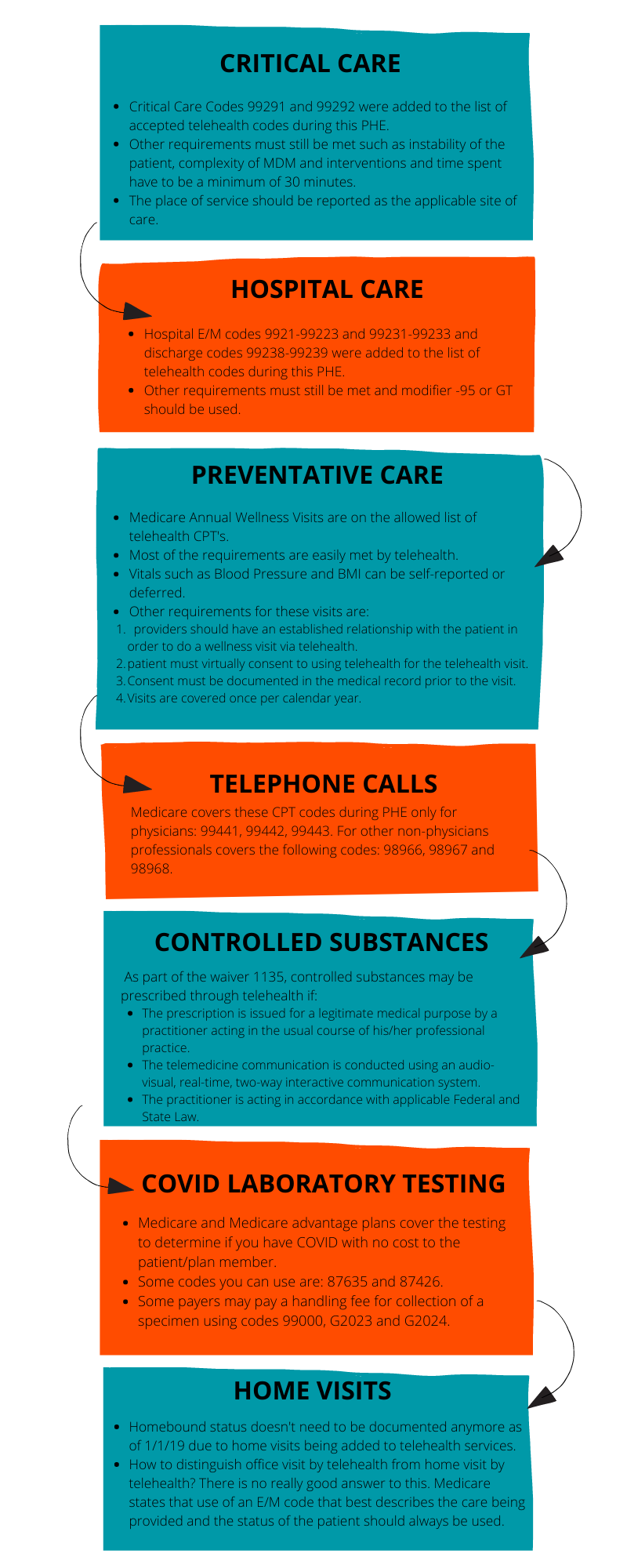
For all visits not related to COVID, you will document and code as normal. According to the Diagnosis Coding Guidelines, you must code all documented conditions that coexist at the time of the encounter, and require or affect patient care, treatment, or management. Effective April 1st, 2020, you have to use ICD10 codes for:
- U07.1 Virus identified and confirmed COVID-19.
- U07.2 COVID-19, virus not identified is assigned to a clinical or epidemiological diagnosis of COVID-19 where laboratory confirmation is inconclusive or not available.
*U07.1 and U07.2 may be used for mortality coding as cause of death.
For suspected cases, code the symptoms or reason to suspect as:
- Z20.828 Contact with and (suspected) exposure to other viral communicable diseases.
- R05 Cough
- R50.9 Fever
It is important that you look at the guidelines for each payer. Don't assume that they are the same as CMS. Remember that documentation still has to fulfill the requirements of the code used and that all diagnosis codes should be documented at each encounter. Make sure to store your encounter information where its accessible for the provider and the payer if a review is needed.
If you have any question or if you want more information, feel free to contact us at: marketing@hpiinc.com. Subscribe to our Health Prime blog to stay tuned on our upcoming webinars and all the latest updates to run your medical practice better so you can focus on what matters the most: your patients.





-3.png)
-3.png?width=380&name=health-prime-logo5%20(002)-3.png)
Submit a Comment