- Run reports to identify the reasons behind your denials, pick one of the core causes at a time and set realistic goals for improvement are some steps you can take to improve your denial rate.
- According to MGMA (Medical Group Management Association), a 5% to 10% denial rate is the industry average.
- Health Prime's benchmark for controllable denials is below 2%.
Approximately 90% of denials within any healthcare organization are preventable. However, medical practices struggle with keeping their denial rate low which turns out having a negative impact on their revenue collection. That is why it is important that you implement a few strategies to reduce denials and make sure you are getting paid for your work.
Before you try to control your denials, you need to identify what's your denial rate. It represents the percentage of claims denied by payers during a given period. This metric quantifies the effectiveness of your Revenue Cycle Management (RCM) processes. If you have a low denial rate, it indicates that your cash flow is healthy and fewer staff is needed to maintain that cash flow.
To calculate your practice's denial rate, you need to add the total dollar amount of claims denied by payers within a given period and divide by the total dollar amount of claims submitted within the given period.
According to MGMA (Medical Group Management Association), a 5% to 10% denial rate is the industry average but keeping the denial rate below 5% is more desirable for your practice. Health Prime's benchmark for controllable denial percent is below 2%. Controllable denials are the denials that can be controlled by improving front end or billing processes.
What can you do to prevent denials?
1. Understand what the true denial reasons are
Deep dive into your denial reports and identify what are the main reasons your claims are being denied. Based on that, you will be able to know where your practice is specifically having issues and then focus on correcting those.
According to an MGMA Stat poll where the association asked healthcare leaders what is the root cause of claims denials/pends in their organization, 36% answered "missing information", 31% reported "prior authorization", 15% said "eligibility", 5% said "out of network" and the other 13% responded "other.
2. Run a report of your top 10-20 denials reasons
Look closely at your reports and you may see some trends. For example, there could be more than one that is related to inaccurate or missing insurance information. There may be several related to authorization or eligibility. Put these into general buckets, and you will likely be left with just a few core causes.
According to an article published on the MGMA, most practices find that 80% of their denials are a result of 20% of the problems.
3. Pick one of your core causes
Select one of the main causes that you found is increasing your denial rate. Maybe you will choose to focus first on missing information. Once you have that selected, you can make a plan to reduce those denials.
Work through your core issues one at a time and set a realistic goal for improvement. If your current denial rate is 12%, you might start cutting that to eight percent over the next six months.

Make sure that you set a SMART goal. SMART is an acronym that you can use to guide your goal setting. Using this technique will help you create clear, attainable and meaningful goals, and develop the motivation, action plan, and support needed to achieve them.
What are some suggestions for the most common
denials reasons?
- Always read back information to the patient or ask them to check it in person at check in. It is easy to transpose an address number or misspell a name. You can correct many small problems by doing this.
- Ideally use online appointments where patients enter their own information to save time for both you and the patient. Many Urgent Care clinics offer the ability to get a same-say appointment online. It's also a great way to help boost your online reputation.
- Confirm eligibility every step of the way. If patients schedule ahead of the appointment, check eligibility at scheduling. Then, check again when they check in. If there's an eligibility problem, you can discuss it with the patient. This also allows you to collect copays at check in. Your practice management system should offer instant eligibility checking.
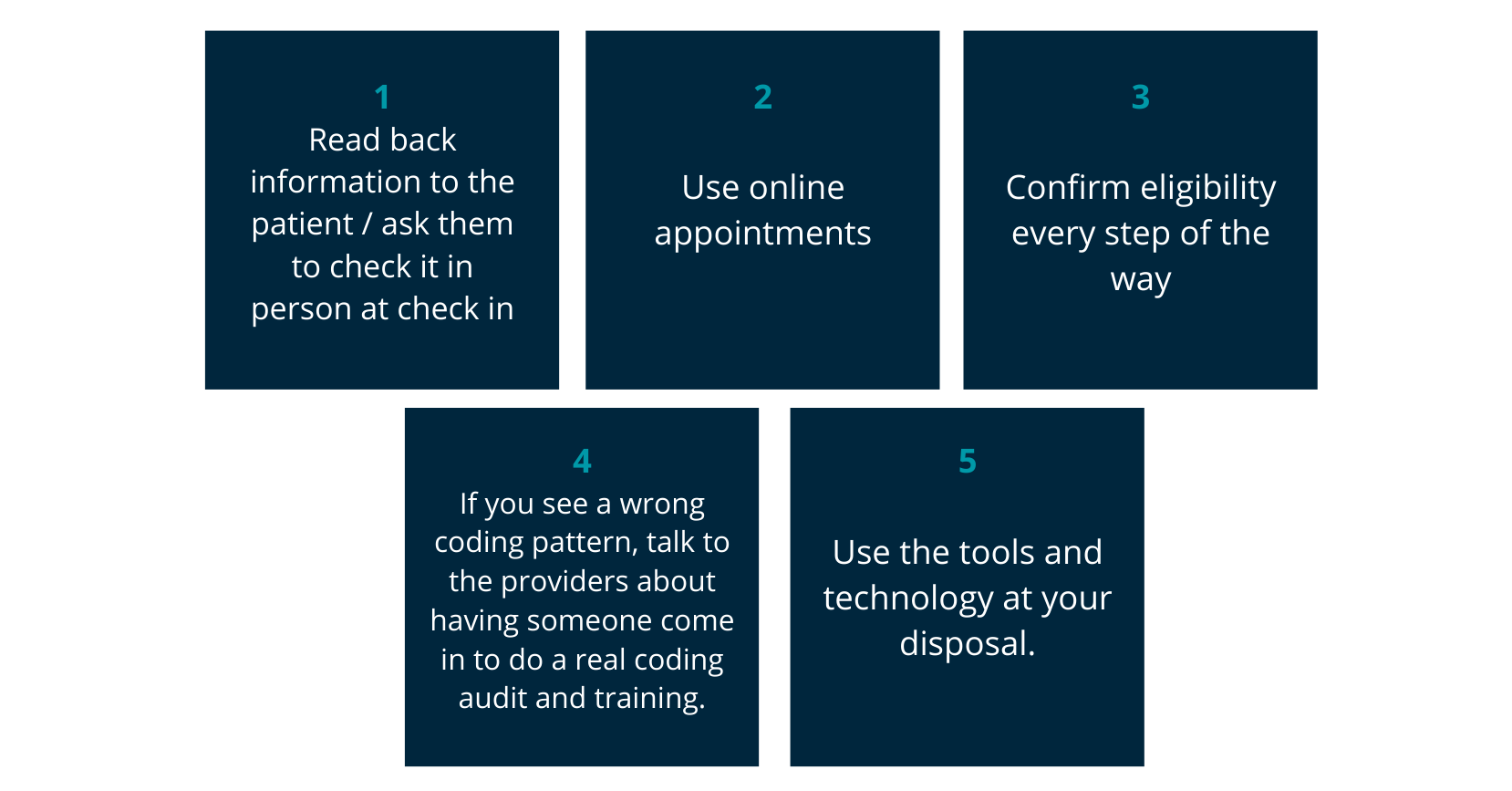
- If you see a pattern of wrong coding, consider talking to the providers about having someone come in to do a real coding audit and some coding training. It can be tricky to talk to providers about coding problems, but it's an important part of ensuring billing accuracy.
You may find that you are not only getting denials but also find that they are under or over coding, which could mean that you aren't getting paid the right amount when you do get paid. Practicing this bad habit could also trigger an audit of your practice. - Use the tools and technology at your disposal. Run denial reason reports. Check in on your progress regularly. Use claim tracking tools to monitor claims and address the denials you do have quickly.
Health Prime's Datalytics, a business intelligence platform that focus on insights that other medical billing solutions neglect, can help you keep track of the reasons behind your denials so you can set an improvement plan for your medical practice. To know more about it, subscribe to our Datalytics blog.
The important thing with denials is to understand what is causing them and then one by one fix the problems. Don't try to tackle every problem at once. It's tempting but it might be too much to manage and will be less effective that working on each core reason at a time.
Ultimately what you want is a long-term reduction in denials and improvement of your aged A/R. Achieving that best practice metric of 2% denial rate or less is truly a case of slow and steady improvement that will win that race.
At Health Prime we understand the importance of reducing your denial rate and keeping it under control so you can optimize your practice, increase revenue, and ensure that you get paid for your work.
If you want more information about how to reduce your denial rate, feel free to email us any question you may have at marketing@hpiinc.com. Set up a meeting with us to discuss how Health Prime can help you get your practice back in its prime.
Subscribe to our Health Prime blog to stay tuned on all the latest updates to run your medical practice better so you can focus on what matters the most: your patients.





-3.png)
-3.png?width=380&name=health-prime-logo5%20(002)-3.png)
Submit a Comment